Heart Transplant
Overview
A heart transplant is an operation in which a failing, diseased heart is replaced with a healthier, donor heart. Heart transplant is a treatment that's usually reserved for people who have tried medications or other surgeries, but their conditions haven't sufficiently improved.
While a heart transplant is a major operation, your chance of survival is good, with appropriate follow-up care.
When faced with a decision about having a heart transplant, know what to expect of the heart transplant process, the surgery itself, potential risks and follow-up care.
Why it's done
Heart transplants are performed when other treatments for heart problems haven't worked, leading to heart failure. In adults, heart failure can be caused by several conditions, including:
- A weakening of the heart muscle (cardiomyopathy)
- Coronary artery disease
- Heart valve disease
- A heart problem you're born with (congenital heart defect)
- Dangerous recurring abnormal heart rhythms (ventricular arrhythmias) not controlled by other treatments
- Amyloidosis
- Failure of a previous heart transplant
In children, heart failure is most often caused by either a congenital heart defect or a cardiomyopathy.
Another organ transplant may be performed at the same time as a heart transplant (multiorgan transplant) in people with certain conditions at select medical centers. Multiorgan transplants include:
- Heart-kidney transplant. This procedure may be an option for some people with kidney failure in addition to heart failure.
- Heart-liver transplant. This procedure may be an option for people with certain liver and heart conditions.
- Heart-lung transplant. Rarely, doctors may suggest this procedure for some people with severe lung and heart diseases, if the conditions aren't able to be treated by only a heart transplant or lung transplant.
Factors that may affect your eligibility for a heart transplant
A heart transplant isn't the right treatment for everyone. Certain factors may mean you're not a good candidate for a heart transplant. While each case is considered individually by a transplant center, a heart transplant may not be appropriate if you:
- Are an advanced age that would interfere with the ability to recover from transplant surgery
- Have another medical condition that could shorten your life, regardless of receiving a donor heart, such as a serious kidney, liver or lung disease
- Have an active infection
- Have a recent personal medical history of cancer
- Are unwilling or unable to make lifestyle changes necessary to keep your donor heart healthy, such as not drinking alcohol or not smoking
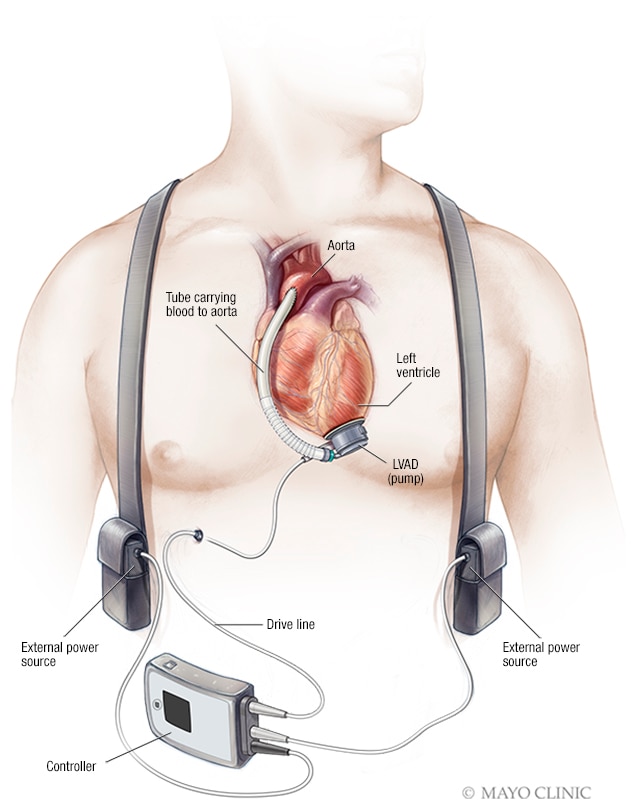
Ventricular assist devices
-
Left ventricular assist device (LVAD)
For some people who can't have a heart transplant, another option may be a ventricular assist device (VAD). A ventricular assist device is a mechanical pump implanted in your chest that helps pump blood from the lower chambers of your heart (ventricles) to the rest of your body.
VADs are commonly used as a temporary treatment for people waiting for a heart transplant. These devices are increasingly being used as a long-term treatment for people who have heart failure but aren't eligible for a heart transplant. If a VAD doesn't help your heart, doctors may sometimes consider a total artificial heart — a device that replaces the ventricles of your heart — as an alternative short-term treatment while you're waiting for a heart transplant.
Risks
Complications of surgery
Heart transplant surgery requires open heart surgery, which carries the risk of many complications, including:
- Bleeding
- Infection
- Blood clots
- Heart attack
- Stroke
- Death
Risks of having a heart transplant
Although receiving a donor's heart can save your life, having a heart transplant has many risks. Risks include:
- Rejection of the donor heart. One of the most significant risks after a heart transplant is your body rejecting the donor heart.Your immune system will see your donor heart as a foreign object that's not supposed to be in your body. Your immune system will try to attack your donor heart. Although all people who receive a heart transplant receive immunosuppressants — medications that reduce the activity of the immune system — about 10 percent of heart transplant recipients still have some signs of rejection that need treatment during the first year after transplantation. This is often effectively treated with medication.Usually the rejection is without any symptoms and requires only an adjustment of medications. If you miss doses of medications, however, the rejection can be severe and very serious. It's important that you follow the instructions as explained by your doctors.To determine whether your body is rejecting the new heart, you'll have frequent heart biopsies to test your heart tissue during the first year after your transplant. After the first year, the number of biopsies is significantly reduced.
- Problems with your coronary arteries. After your transplant, it's possible the walls of the arteries in your heart (coronary arteries) could thicken and harden, leading to cardiac allograft vasculopathy (CAV). This can make blood circulation through your heart difficult and can cause a heart attack, heart failure, abnormal heart rhythms (arrhythmias) or sudden cardiac death.Your doctor may recommend annual tests after your transplant to monitor your coronary arteries for CAV.
- Medication side effects. The immunosuppressants you'll need to take for the rest of your life may cause kidney damage and other problems. Other complications of these medications can include high blood pressure, high cholesterol, diabetes and a condition in which your bones become thin and weak (osteoporosis).
- Cancer. Immunosuppressants can also increase your cancer risk. Taking these medications can put you at a greater risk of skin cancer, non-Hodgkin's lymphoma and other solid tumors. Regular checkups are necessary to detect the development of cancer.
- Infection. Immunosuppressants decrease your ability to fight infection. Some heart transplant recipients may develop an infection that requires them to be admitted to the hospital during the first year after their transplant. The risk of infection decreases over time as the amount of immunosuppressant medication is decreased.
Submit your abstracts and register for the GLobal congress on Cardiology and Interventional Cardiology and share you research in the field of Cardiology.
Website: https://goo.gl/BbtGC2

Comments
Post a Comment